Stages of psoriasis are defined time intervals during which the disease acquires its characteristic features. Many patients with psoriasis mistakenly refer to the stage as a severe or mild form of the disease, but the term is used in medical documentation in a completely different sense.
What are the stages of psoriasis?

Psoriasis is a recurrent skin pathology in which genetics are at fault. Dermatologists say at least 2% of the world’s population suffers from this disease, which means the problem is very urgent. During psoriasis, 2 states are clearly distinguished:
- Relapse.This term refers to skin deterioration. In the event of relapse, the patient suffers from itching, pain, burns, profuse skin eruptions, irritation, and discomfort. The victim's situation is exacerbated by insomnia, neurosis and anxiety.
- Remission.This word is used to improve the appearance of the skin. With remission, the skin regains its normal color, the redness disappears, and the area of psoriasis plaques decreases.
The stages of psoriasis partially repeat the descriptions of remissions and relapses, so many dermatologists use these words alternately. In clinical practice, 3 stages of psoriasis are described:
- progress stage;
- standing;
- regression phase.
Considering that we are talking about a cyclical process, the stages flow one after the other and form a continuous course of the disease.
Fact!The stage of progress is considered to be the most difficult to feel.
What is the progression of psoriasis?
The stage of progress is triggered by a number of triggers, such as the cold season or stress. In some cases, even an experienced dermatologist cannot clearly determine the cause. In the progressive phase, the following happens:

- Psoriatic nodules develop rapidly, affect the skin, and connect in so-called plaques that peel and itch. A plaque is a patch of any shape, most often round or oval, sometimes with an uneven edge.
- Papules, or lumps in the rash of psoriasis, are lumps on the skin. The edges of the papules do not peel off and the middle part is peeled off. As a large number of dead scales accumulate, plaques begin to rise above the surface of the skin. Puffiness gives them an even more convex and uneven look.
- This stage of the pathology is characterized by an isomorphic reaction consisting of exacerbation of rashes, scratches, injections, cuts, and microtraumas with skin lesions. This phenomenon is called Köbner.
Delayed response is characteristic of the progressive stage of psoriasis. In some cases, the rash occurs about a day after exposure to the trigger (e. g. , a food allergen). Typically, a psoriasis rash appears within 24 hours of exposure to harmful factors.
Interesting!95% of patients with psoriasis have some type of food intolerance that can cause a relapse. To avoid aggravation, you should keep a food diary and monitor your reaction to different types of food.
Stationary and recessive sections
The inpatient phase is the process of psoriasis, during which the victim's condition relatively stabilizes. In the stationary section:

- Psoriasis plaques have a smooth outline. The entire surface of the plaque is covered with a thick layer of scales that peel off easily. The itching and discomfort is moderate. There is no bright red inflamed rim around the papules.
- With skin microtraumas, the Koebner phenomenon is not observed, i. e. scratching or cutting off healthy skin no longer becomes a psoriatic plaque.
The regressive or recessive stage is characterized by severe lesions of psoriasis. First, a pseudo-atrophic rim is seen around the papules, and then patients notice a rapid cessation of exfoliation of the skin, with hyperpigmentation plaques forming in its place.
Severity of pathology
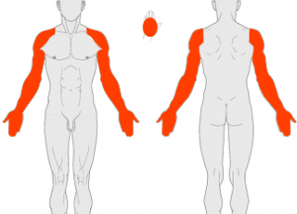
Another diagnostic criterion is to evaluate the area of psoriatic lesions. The term "severity" is used to describe it. Dermatologists distinguish between 3 degrees of skin disease:
- Easy.Psoriatic plaques occupy 1-3% of the total body area. The small size of the affected areas does not mean that the patient would benefit. With psoriasis of the head or face, even a few plaques are enough to cause discomfort and torment to a person.
- Medium.Outbreaks of psoriasis account for 3 to 10% of the total body area. In this case, the back, chest, and outer surfaces of the joints, scalp, palms, and legs are affected. This prevalence leads to severe poisoning and severe pain. The patient may lose all or part of his ability to work, and his mental and nervous system may deteriorate.
- Difficult.The disease covers more than 10-15% of the skin surface. It is roughly estimated that if psoriasis occupies more than a quarter of the total body area, the likelihood of liver or kidney failure increases many times over. Decompensated damage to internal organs can cause death in patients with psoriasis.
A special scale called PASI is used to comprehensively assess the severity of psoriasis. The scale takes into account:
- percentage of healthy and diseased skin
- ; the
- stage of the pathology;
- patient's response to drug therapy;
- individual tolerance of psoriasis (mental state, nervous system and psyche complications);
- Objective data from laboratory tests in dynamics (e. g. , amount of uric acid in a blood test).
The diagnosis takes into account all the symptoms that affect the condition of a person with psoriasis. The intensity is reflected in the medical record:
- itchy processes of the skin;
- redness;
- swelling;
- hyperemia;
- thickening of the skin;
- exfoliation;
- blood flow;
- swelling;
- infections;
- pain syndrome.
On the PASI scale, the volume of skin lesions is described by numbers, from 0 to 72, where 0 is the absence of skin symptoms and 72 is the highest possible maximum spread of the disease.
Attention!First, it is important for the patient to know and watch for signs of exacerbation. If you experience any adverse symptoms, you should see a dermatologist immediately because psoriasis does not always enter the standing stage itself. The downturn can last for decades.
Treatment of psoriasis depends on the stage
A set of therapeutic measures has been developed for each stage of the disease, so the dermatologist’s first task is to determine if the psoriasis is progressing, stabilizing, or regressing.
How to handle the progressive stage
Every person with psoriasis thinks that remission ends based on their own feelings. If the itching gets worse, the skin looks worse, and the psoriasis is obviously spreading to the surface of the body, treatment should be started. Advanced therapy has the following characteristics:
- The patient deals with the prevention of further deterioration, strictly adheres to the diet, refrains from the causes of the pathological process (stress, smoking, alcohol).
- In case of severe itching, antihistamines can be used, another advantage of this group of drugs is the removal of swellings in the area of psoriasis plaques.
- A dermatologist prescribes a wide range of topical treatments to heal, soften, and thin the skin. Creams, ointments or sprays are selected at the discretion of the physician. Tar soap and solid oil compaction give positive dynamics. You can also use compaction or cosmetics with Dead Sea mud.
At this stage, the main task is to stop the exacerbation before the disease comes into prolonged relapse. According to the indications, the doctor selects corticosteroids by injection or as an ointment.
Attention!Corticosteroids should be used in short and intensive courses under the supervision of a dermatologist. You can give yourself injections or smears with antihistamine ointments.
Inpatient and regressive therapy

The dermatologist's further actions depend on the body's response to the treatment chosen. The following scenarios are possible:
- Medication has a positive effect. Within 1-2 weeks, the psoriasis passes through the standing area, regresses, and remission occurs.
- Medicines have no effect. If, 2 to 4 weeks after prescribing the medication, the results are still not visible, this justifies changing the list of medications or your doctor.
- The drug is aggravated. Such dynamics are also possible, especially if the dose or frequency of administration is insufficient. The relapse is delayed, the plaques of psoriasis cover a large area of the body, the person needs hospital treatment.
A medical institution uses more powerful therapy, such as hardware blood purification. With a favorable reaction, psoriasis enters a stationary phase that can last from several days to several months.
Interesting!More than 80% of patients notice the seasonal nature of exacerbations. This makes the disease predictable and allows you to prepare for the onset of relapse.
The list of inpatient and regressive drugs is exactly the same, but dosing and dosing frequency are lower than in the progressive phase.
10-15 year remission
The competent dermatologist has set himself the task of selecting drugs and physiotherapeutic agents that will result in the longest possible improvement for patients with psoriasis. In this case, the patient himself should do everything possible to facilitate the treatment, avoid the root causes, and take the medication responsibly. If the alliance between the patient and the physician is successfully established, the duration of remission is unlimited. Stable wellness can last for at least 15 years.























